Back Pain in Pregnancy: Causes, Symptoms and Treatments
* For the purpose of this blog, we will be referring to those who can child-bear as female-born. We are committed to ensuring we are inclusive to all those who experience pregnancy.
Let’s dive deeper into back pain and look at one major presentation type that we see here at Viva Physiotherapy – Back Pain during Pregnancy.
Finding out that you’re expecting can be an overwhelmingly exciting, and sometimes daunting, time. You may start to rollercoaster through some changes involving your mood, energy, mindset, sleep and appetite. Your body will also begin to work through many incredible changes to start to nourish your child and allow for the growth within you. Though this time can be trouble-free for some, others may face some challenges along the way.
Although these emotional, physiological and anatomical changes are natural, there can be common and sometimes unwanted musculoskeletal imbalances related to stability, hormones and changes in body shape. One of the biggest complaints during pregnancy is lower back pain. In fact, it is estimated that more than 50% of women experience some degree of backache throughout their pregnancy. There can be numerous reasons for the onset, or severity, of back pain, so let’s dive deeper into that..
What to expect
- Why does my back hurt?
- What are the common types of back pain that we see?
- Causes for back pain during pregnancy
- Understanding the biomechanical influences of back pain
- Understanding the hormonal changes through pregnancy
- Have back pain in pregnancy – so what should you do about it?
- Tips on how to reduce back pain whilst sitting
- Tips on how to reduce back pain whilst sleeping
- Stretches for back pain relief during pregnancy
- How can I prevent the onset of lower back pain during pregnancy?
Why does my back hurt?
As you may be familiar with, there are many changes to your body that occur during pregnancy. Due to some of these changes, you can be at higher risk of developing back pain than the regular person. Although it is common, it is certainly not normal, and there is a lot we can do about it. First, let us help you understand why you might be experiencing back pain.
It is important to first and foremost understand how we, as humans, experience and perceive pain. Pain is a personal experience for each individual (Bachman, 1995). Factors such as cultural and social circumstances, counter-stimuli, fear and anxiety, personality, fatigue, expectations, and distraction from pain can affect how a person perceives and copes with pain (Bachman, 1995; Bevis, 1993). Pregnancy-related side effects have been reported more frequently in younger pregnant women, alluding to the fact that age is an important factor which can alter pain perception (Greenwood & Stainton, 2001). There has also been links to show that those who experience more stress in their daily lives (for example within their occupation) will report higher severity of back pain during pregnancy.
With influences of pain and pain perception in mind – it is also important to note that the origin and cause of back pain during pregnancy is a little uncertain, and is probably multifactorial (Bo et al., 2016). Let us first explain the different areas of back pain that we see.
What are the common types of back pain that we see?
Upper back pain
Upper back pain occurs in the region of your spine between the base of your neck, and the bottom of your ribcage. This is the region of your thoracic spine. Pain here can often be attributed to postural changes, reduced mobility through the spinal joints, tension through the muscles, and changes in the ribcage as the bump grows bigger. There are many different strategies that can assist with management of pain in the upper back.
Middle back pain
Middle back pain is used somewhat interchangeably with upper back pain. It again refers to pain within the thoracic spine region, however mostly in the middle part of your back (quite literally!). Within this region, women can also often experience some rib pain – this can be from the movement that occurs at the joint of the ribs to the thoracic spine, or can alternatively be pain referred from the middle back itself.
Lower back pain
Lower back pain is defined as pain between the 12th (or lowest) rib and the gluteal fold (the fold underneath your buttock), with or without leg pain. It is the area just above your buttock really, with lower back pain affecting most people at least once in their life, and approximately 50% of people throughout pregnancy (Katonis et al., 2011).
Pelvic girdle pain
European Guidelines have defined pelvic girdle pain as pain experienced between the back of the pelvis and the gluteal fold. This pain can radiate down into the back of the thigh, and also occur anteriorly at the pubic bone region. In terms of differentiating between lower back pain and pelvic girdle pain, a Physiotherapist can examine you to achieve a correct diagnosis.
For the purpose of this blog, we will be delving further into the most common type of presentation – lower back pain.
Causes for back pain during pregnancy
Back pain can occur during pregnancy for a number of different reasons. Historically, the main causes were categorised into two main categories: biomechanical changes and more systemic, or hormonal changes, affecting the dynamic stability of the pelvis. However, recent evidence supports the notion that pain experienced during pregnancy is much more multifaceted than initially thought, and in fact has no correlation to the hormonal changes that occur.
According to the Australian Government Department of Health and Aged Care, the risk factors for developing lumbopelvic pain during pregnancy include:
- History of lower back pain or pelvic girdle pain
- Increased number of previous pregnancies
- Physically demanding work
- Work dissatisfaction
- a high body mass index (BMI)
- Emotional distress, depression and/or anxiety
- Smoking
- A belief that pain will not improve
- Fear avoidance
- Previous pelvic trauma
(Albert 2006, Bjelland et al., 2010; Fernando et al., 2020; Robinson et al., 2010; Morgren, 2005; Eberhard-Gran & Eskild, 2008)
Understanding the biomechanical influences of back pain
Though the biomechanical changes that occur during pregnancy are all expected and necessary, and will not necessarily determine whether you experience back pain or not, it remains important to understand these changes and how they may impact you.
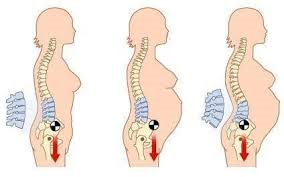
Biomechanics refers to the way our body moves and holds itself (like posture). Overall, mechanically, we expect changes within the pregnant body to adapt to the increasing weight of the enlarging uterus and its contents. As the uterus expands and grows, the centre of gravity shifts forward, and we see increased extension into the mid to lower back. Simply put, the pregnant belly needs to grow away from the body, a process in which the lumbar spine is pulled forward with it, increasing the inward curve (or lordosis) of the lower back. There is also stretching of the surrounding tissues both mechanically and due to hormones, which adds to the resultant posture changes. These postural changes are all a normal and important part of the human body to adapt to the baby, hence it can be expected for each child-bearing person. They are natural, necessary, and safe. They can however, for some people, be a contributing factor to some pain experienced in the lower back. Due to the altered equilibrium of the spine, you may experience pain due to the compression of the vertebrae, the altered load on the ligaments, or the shortening of the lower back muscles.
Other musculoskeletal implications on the body include the stretching and weakening of abdominals, the possible weakening of the pelvic floor muscles due to the increased load, and the potential inhibition of gluteal (or buttocks) muscles due to altered posture. Outside of the lower back, there can also be effects on the upper body such as tightness into pectoral (chest) muscles, inhibition of the neck stabilising muscles, and overactivity in the more superficial neck muscles (Fiat et al., 2022; Greenwood & Stainton, 2001; www.parents.com)
Understanding the hormonal changes through pregnancy
In addition to the physical changes, are the changes in hormones throughout pregnancy. Two hormones in particular, progesterone and relaxin, increase significantly during pregnancy and have a profound effect on the body. These hormones both allow for the relaxation and stretching of ligaments and tissues within the body to allow for the growing baby. As these hormones circulate throughout your entire body, it can cause loosening and instability in all joints, hence it was previously thought that this would leave them prone to painfully imbalanced alignment or even injury. However, most recent evidence shows that there is in fact no relationship between the level of relaxin and the experience of lower back or pelvic girdle pain. The changes are normal, safe, and necessary, and do not lead to the onset of pain that may be experienced.
Let us explain some of these hormonal changes in more detail at the different stages of pregnancy, and their effects on the body.
1st Trimester(H3)
This trimester is from conception to 12 weeks. Although you may not look pregnant during the first trimester, your body is going through enormous changes as it accommodates your growing baby. Your hormone levels will change significantly in the first few weeks following conception. The hormone progesterone increases exponentially during the first 10 weeks of pregnancy, and then reaches a plateau. High levels of this hormone help relax the muscles (including the uterus) and the ligaments surrounding the pelvis. Simultaneously, another hormone, relaxin, reaches its peak at around 12-14 weeks of pregnancy – having similar effects on the body.
2nd Trimester
By the second trimester, at 12 – 27 weeks, the uterus continues expanding as the foetus grows more rapidly. It may be during this trimester that you start to notice physical changes within your body as your foetus increases about six times in size. During this trimester, postural changes, weight gain, and potential muscle separation can become more apparent. The hormones relaxin and progesterone have reached their peak, and although they have positive effects on the ability of your body to tolerate the growing belly, there are natural, yet sometimes unwanted side effects on the body overall. You may find that you begin to notice some separation through the centre of your abdominal muscles – a term known as Diastisis of the Rectus Adbominus Muscles, or DRAM. You can read more about DRAM later on in this blog.
These changes will really overlap with those in the 3rd trimester, so read below for more!
3rd Trimester
The third trimester begins at week 27, and ends at birth. During this trimester is when the body changes are most pronounced in the weeks leading up to birth, with the foetus growing ever-more rapidly. Again, like the second trimester, this is where weight gain, postural changes and potential muscle separation, or progression of, can impact the body.
At approximately week 31 of pregnancy, your baby has finished most of his or her major development. Now it is time for them to gain weight – quickly. Hence, during this time, you will notice your bump growing rapidly. Again, with the change in body shape, you will find that your centre of gravity is shifting further forward. If your body does not have the strength to counteract this, this will lead to further extension into the lower back, compression on the joints, and shortening of the lower back muscles – all of which can contribute to pain (Greenwood & Stainton, 2001).
Later in the third trimester, you will again experience another surge in the hormone relaxin in order to prepare your body for labour. A few days before labour, you may notice looser, more relaxed joints in your pelvis and lower back, as the hormone helps relax the pelvis to allow your baby to descend the birth canal (www.parents.com). Nothing to worry about though – it’s just your wonderful body getting you ready for the birth!
So, you may have back pain in pregnancy – so what should you do about it?
How best to manage back pain during pregnancy and when to seek help
Firstly, it is important to recognise that there are in fact plenty of strategies and ways to improve your back pain during pregnancy. Early intervention for pregnancy-related back pain can be very beneficial in order for you to make sense of your pain experience, and obtain education on how best to manage it throughout your pregnancy. In order to combat back pain, we need to look at and address the individualised potential causes as to why you may be experiencing back pain and ensure we manage it with a multimodal and holistic approach.
Reframing beliefs about back pain
Firstly, it is important to understand that your body is not falling apart! The changes that your body is going through are certainly normal, safe and necessary for the pregnancy journey. It is now more broadly understood that pelvic girdle and lower back pain during pregnancy is more a reflection of the sensitivity of tissues, and not tissue instability, injury or harm. Hence, it is important to understand and reflect on your pain in a more holistic way, and restructure your beliefs and fear surrounding pain. New evidence has shown that the strongest predictor of resolution of pregnancy-related pelvic girdle and back pain is having the belief that it will go away (Pulsifer et al., 2022).
Self-management
As pain onset and intensity are influenced by the stress response system, emotional wellbeing, and sleep quality, these are all aspects of care that can be influenced to positively impact on your pain experience. Self-care strategies such as optimising sleep and emotional wellbeing, exercise, and surrounding yourself with external support can all be effective in the management of pain. Individualised pain education can also help combat pain, so don’t be afraid to talk about this more with your health professional (Pulsifer et al., 2022).
Postural awareness
It is important for you to have awareness of the natural postural changes that will occur during pregnancy, in order to understand how your body may respond, and how you can improve on this if it is contributing to your pain. Often, women find that lower back pain may be worse with prolonged sitting or standing, which is likely attributable to the posture you are adopting. We work closely with people at Viva to build awareness into their static and dynamic posture, in order to help combat pain. Follow along below for a little more insight into this!
Tips on how to reduce back pain whilst sitting
Sitting posture is important for every person, especially for those who spend a lot of time sitting. It is then particularly important for pregnant women, as we know there is already an increased load on the body. Let us work through how to best find your active sitting position to give you the best chance of being pain-free whilst seated.
Firstly, I want you to begin your body scan at your pelvis. Are you sitting nice and tall on your sitting bones, or are you perhaps slouching back and sitting passively through the pelvis?
I would like you to do a few pelvic tilts to check on this. I want you to imagine your pelvis as a fish bowl full of water. I want you to tilt your pelvis to ‘tip water out the front of the bowl’, then I want you to reverse this and ‘tip water out the back of this pelvic bowl’. As you’re doing this you should start to feel some awareness and activation into your lower, deep abdominal stabilising muscles. Then, I want you to find the centred position so your pelvic ‘fish bowl’ is nice and centred. This is the foundation of your sitting (and standing) posture. If you want more practice of this you check out out video ‘How to Sit Actively‘.
As much as possible, it is important to remain ‘active’ in sitting posture when you can – though of course our body will get tired and fatigued in doing so regularly throughout the day. If you can, each hour you should check in on your sitting posture and begin the hour with a nice active sitting position. Then, once your body feels fatigued, you want to support yourself up in this position for the remainder of the hour using the back of the chair, and things such as a rolled up towel (or lumbar support) right at the base of the spine.
Other things to look at in sitting position, particularly for pregnant women, is to make sure that hips are higher than knees when sitting, and that things such as your computer screen are at the level of your eyes, so as not to slouch whilst sitting.
Tips on how to reduce back pain whilst sleeping
There can be positioning tips during sleep that can help reduce pain. Firstly, ensuring you have a pillow between your knees can assist in keeping your pelvis supported, and also helps prevent the onset of outer hip or thigh pain. Then, things such as a cushion underneath your lower ribs in side-lie, and a pillow underneath your bump can help support you further.
Physical activity and strengthening
In order to tolerate the increasing load that pregnancy puts on the human body, it is strongly recommended that you adopt and/or continue exercise during pregnancy.
Exercise guidelines for pregnant women now very much encourage exercise throughout pregnancy, in the absence of certain contraindicated medical concerns. As per the Australian Department of Health, the Physical Activity and Exercise Guidelines explicitly state that pregnant women should be partaking in physical activity most days of the week, to a weekly total of either:
- 2.5 to 5 hours of moderate intensity physical activity
- 1.25 to 2.5 hours of vigorous intensity physical activity
- An equivalent combination of moderate and vigorous activities
It is also explicitly stated that this should include at least 2 days of muscle strengthening exercise each week as well as pelvic floor exercises. Any form of movement though, is better than nothing. So don’t put too much pressure on yourself if you’re not able to quite hit these specific targets.
Studies have shown that compared with not exercising, when following and meeting exercise guidelines, prenatal exercise can decrease the severity of lower back pain and/or pelvic girdle pain during and following pregnancy (Bo et al., 2016; Davenport et al., 2019; Gjestland et al., 2013; Pennick & Liddick, 2013). The European guidelines for pelvic girdle pain (2008) recommend specific stabilising exercises including local and global muscle systems as a treatment for pain (Vleeming et al., 2008). However, more recent recommendations now focus on empowering women to move in diverse and novel ways that are comfortable for them, regardless of the specificity of the exercises (Pulsifer et al., 2022; Clifton et al., 2017). It is much like training athletes with pain in the absence of acute trauma or injury – there is a need to create more freedom, flexibility, strength and diversity of movement – all of which allow for more comfort and resiliency (Pulsifer et al., 2022). If you would like to read more about the benefits of movement, and particularly pilates during pregnancy, read our post titled ‘10 Benefits of Doing PIlates When You’re Pregnant‘.
There are, however, some forms of exercise that should be avoided, particularly once women are into their second or third trimesters. These include exercise on their back and exercises which shorten through the abdominal muscles (such as crunches/sit-ups and roll downs). Exercises should also be individually tailored according to the woman throughout the course of her pregnancy. For example, if someone is experiencing back or pelvic girdle pain, we will alter single-leg stance exercises according to their symptoms. To view an example of a pre-natal appropriate class, see our Stay Fit in Pregnancy Class or you can read more about our Stay Fit in Pregnancy Classes.
Stretches for back pain relief during pregnancy
If you are already experiencing pain, there are certainly numerous exercises and stretches that can help relieve this for you. Examples of some of these that have proven to benefit pregnant women are:
- Thread the needle
- Cat-Cow stretch
- Rockbacks (feet wide, and feet narrow)
- Hip flexor stretch in kneeling
Need more explanation? We have a video explaining the exercises.
What’s the role of the pelvic floor in all of this?
So, I’m sure if you are pregnant, or planning to start a family in the near future, you’ve probably heard all the hype about the pelvic floor. But what is it, and what is the role of it in all of this?
Well, we picture the pelvic floor as the imaginary bottom of our core ‘canister’, or coke can, if you can picture that better. The pelvic floor is a sling of muscles that spans the pelvis from front to back, and also side to side. It supports all of our pelvic organs, has a big role in continence and sexual health, but also provides a lot of support and stability to the core of our body. Through research, we know that if there is a weakness or dysfunction in your pelvic floor – whether that be from weak muscles, or perhaps overactive muscles – then this can potentially become a weak link leading to pain. It is important for you to know that the pelvic floor will play a role in supporting your spine during pregnancy (and beyond), and hence very powerful to know that you can activate and train them well. This is something that we can help you a lot with here at Viva! You can read more about the pelvic floor and how we can help here.
Physiotherapy in-room treatment
There is more and more evidence surfacing supporting the use of manual therapy as a safe treatment to effectively treat lower back pain. Within our consultations with pregnant women, we are often providing hands-on treatment including soft tissue massage, deep tissue work, and joint mobilisations to reduce pain and stiffness. We have equipment here such as the bump pillow which allows you to be able to safely lay on your stomach (which can be relieving on its own!) so that we can effectively treat your pain. Learn more about how we can help you throughout this pregnancy journey.
How can I prevent the onset of lower back pain during pregnancy?
You may be reading this as someone who is yet to start a family, and want to know how to prevent back pain from coming on in the first place. Well, there is again a lot that you can be proactive about in order to fend off pain onset.
Firstly, it is important to adopt a healthy lifestyle leading up to planning for pregnancy. This is not only from a physical perspective, but in all aspects of your life. It is important to recognise the impact that biological, psychological and social factors have on your body and your health, and act to optimise these areas of your life leading up to pregnancy. This can be things such as making sure you have a healthy support network surrounding you, making sure you optimise your sleeping pattern as best as you can, and working to eradicate any unnecessary stressors in your life.
In addition to this, ensuring that your physical body has the strength behind it to tolerate and thrive during pregnancy is equally important. If you are not currently a regular exerciser, it is recommended that you try to adopt some form of activity throughout your week to begin to build your cardiovascular fitness, and muscle strength. Working toward meeting the Australian Government physical activity guidelines is greatly beneficial – which will then make it much easier to continue on with into, and beyond, pregnancy.
How does abdominal separation relate to back pain during and after pregnancy?
You may have heard from your health professionals throughout the journey about the word “DRAM” which stands for Diastisis of the Rectus Abdominus Muscle. A DRAM is a separation or stretching of the connective tissue through the centre of your abdominal muscles. It is a common and expected change during pregnancy to allow for the growth of your bub, with up to 66-100% of women experiencing this during their third trimester (Benjamin et al., 2014). There is a lack of consensus on what is normal separation, but generally we see up to 3-4 fingers width separation during pregnancy, which will often return to just a 1 centimetre gap 6 weeks after giving birth.
In some women, this separation can progress a little more than expected. This can be due to various reasons, such as multiple pregnancies (especially in quick succession), excess uterine fluid, a small torso or pelvis, and overuse of the abdominal muscles against resistance during pregnancy, to name a few. Something to watch out for is ‘doming’ at the abdominals during pregnancy, and ensuring you avoid this to prevent overstretching of these tissues.
So yes, the stretching that occurs at the abdominals can on occasion progress a little further than expected, or wanted. This progression can be something that can weaken your core stability and support, and hence attribute to some pain you may be experiencing. The most important thing is that you can develop tension across your abdomen – as this then helps with load transference throughout the core and the body – so it is important to check in with your physio who can assess this for you, and advise you on how to best prevent progression, and encourage healing post pregnancy.
Why does my back still hurt postpartum?
So you’ve gotten to the other end of pregnancy (congratulations!!) and still experiencing some aches and pains post birth? I know this can feel frustrating as you expect your body to revert back to pre-pregnancy form – but it can be common for some things to linger.
As you have learnt, there are a number of changes that occur during pregnancy, and a lot of these will take some time to reverse. We often explain to expectant mothers that pregnancy is like a 9 month ramp up, but also a 9 month ramp down afterwards. It will take time for your body to recover after carrying your child, and going through childbirth, as well as the fact that there are ongoing hormonal changes that will continue even after childbirth. It will also take time for your body to regain strength that you may have lost along the way. It is important for you to make sure you take time to let your body heal, and then gradually return to your normal activities.
Postpartum graduated return to exercise is important, in order to build up your core strength again, which will act as a protector against back pain. We often recommend doing this following your Physiotherapy check in at 6 weeks postnatal, as it is common for women to do too much in the early days, which can put your pelvic floor at risk. Even if you were not a regular exerciser prior to pregnancy, it remains important for you to ensure you rehabilitate your body properly following pregnancy to regain strength, and future-proof your body against the loads of parenthood as well.
In summary:
So, hopefully you feel you have a much better understanding of what can be expected during pregnancy, and some initial strategies you can adopt to help make sense of your pain, and improve it. Just know that yes, your body will certainly go through many different changes throughout this journey, all of which are natural, necessary and safe. Yes, you may experience some discomfort and pain throughout the different stages of pregnancy, but there’s certainly a lot you can do about it, and you shouldn’t just expect to ‘deal with it’ for the remainder of your pregnancy.
We at Viva Physiotherapy are here to help along the way – so please book in for your Initial Pregnancy Appointment to help get you feeling on track for a healthy and enjoyable pregnancy. You can use the code ‘PREGBLOG’ for $20 off this appointment.
References
Albert HB, Godskesen M, Korsholm L & Westergaard JG. (2006). Risk factors in developing pregnancy-related pelvic girdle pain. Acta Obstetric Gynecology Scandinavia, 85(5), 539-544. https://pubmed.ncbi.nlm.nih.gov/16752231/
Benjamin DR, van de Walter ATM, & Peiris CL. (2013). Effects of exercise on diastisis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy, 100, 1-8. https://www.physiotherapyjournal.com/article/S0031-9406(13)00083-7/fulltext
Bjelland EK, Eskild A, Johansen R and Eberhard-Gran M. (2010). Pelvic girdle pain in pregnancy: the impact of parity. American Journal of Obstetrics & Gynecology, 203(2), 146.e11-6. https://pubmed.ncbi.nlm.nih.gov/20510180/
Bo K, Artal R, Barakat R et al. (2016). Exercise and pregnancy in recreational and elite athletes: 2016 evidence summary from the IOC expert group meeting, Lausanne. Part 1 – exercise in women planning pregnancy and those who are pregnant. British Journal of Sports Medicine, 50(10), 571-589. https://bjsm.bmj.com/content/50/10/571
Davenport MH, Marchand A, Mottolla MF, et al. (2019). Exercise for the prevention and treatment of low back, pelvic girdle and lumbopelvic pain during pregnancy: a systematic review and meta-analysis. British Journal of Sports Medicine, 53, 90-98. https://bjsm.bmj.com/content/bjsports/53/2/90.full.pdf
Eberhard-Gran M & Eskild A. (2008). Diabetes mellitus and pelvic girdle syndrome in pregnancy – is there an association? Acta Obstetric Gynecology Scandinavia, 87(10), 1015-1019. https://pubmed.ncbi.nlm.nih.gov/18763174/
Fernando M, Nilsson-Wikmar L & Olsson CB. (2020). Fear-avoidance beliefs: A predictor for postpartum lumbopelvic pain. Physiotherapy Research International, 25(4), e1861. https://pubmed.ncbi.nlm.nih.gov/32568443/
Fiat F, Merghes PE, Scurtu AD et al. (2022). The main changes in pregnancy – therapeutic approach to musculoskeletal pain. Medicina (Kaunas), 58(8), 1115. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9414568/#:~:text=Pregnancy%20produces%20major%20changes%20in,pain%20and%20support%20general%20function.
Gjestland K, Bø K, Owe KM, et al. (2013). Do pregnant women follow exercise guidelines? Prevalence data among 3482 women, and prediction of low-back pain, pelvic girdle pain and depression. British Journal of Sports Medicine, 47(8): 515-520. https://bjsm.bmj.com/content/47/8/515
Greenwood CJ and Stainton MC. (2001). Back pain/discomfort in pregnancy: invisible and forgotten. The Journal of Perinatal Education, 10(1), 1-12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1595051/
Katonis P, Kampouroglou A, Aggelopoulos A, et al. (2011). Pregnancy-related low back pain. Hippokratia, 15(3), 205-210. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3306025/
Mogren IM & Pohjanen AI. (2005). Low back pain and pelvic pain during pregnancy: prevalence and risk factors. Spine, 30(8), 983-991. https://pubmed.ncbi.nlm.nih.gov/15834344/
Pennick V and Liddle SD. (2013). Interventions for preventing and treating pelvic and back pain in pregnancy. Cochrane Database of Systematic Reviews, (8). https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD001139.pub3/full/es
Pulsifer J, Britnell S, Sim A et al. (2022). Reframing beliefs and instilling facts for contemporary management of pregnancy-related pelvic girdle pain. British Journal of Sports Medicine, 56(22), 1262-1265. https://bjsm.bmj.com/content/56/22/1262
Robinson HS, Mengshoel AM, Bjelland EK, Vollestad NK. (2010). Pelvic girdle pain, clinical tests and disability in late pregnancy. Manual Therapy, 15(3), 280-285. https://pubmed.ncbi.nlm.nih.gov/20117040/
Vleeming A, Albert HB, Ostgaard HC, Sturesson B & Stuge B. (2008). European guidelines for the diagnosis and treatment of pelvic girdle pain. European Spine Journal, 17(6), 794-819. https://pubmed.ncbi.nlm.nih.gov/18259783/
https://www.health.gov.au/topics/physical-activity-and-exercise/pregnancy
https://www.health.gov.au/resources/pregnancy-care-guidelines/part-i-common-conditions-during-pregnancy/pelvic-girdle-pain
https://www.parents.com/pregnancy/my-life/emotions/a-cheat-sheet-to-pregnancy-hormones/