Can exercise fix RSI? What I’ve learned from 3 years of treatment

Peer reviewed by Kathryn Anderson, BA Physiotherapy (Honours)
Several months into the pandemic, I was suffering with debilitating pain that travelled from both elbows down through my wrists and into my hands. My desk job was “click heavy”, using both a left- and a right-handed mouse simultaneously to roster (and de-roster!) frontline Aged Care staff and manage hectic inbound call queues. Thanks, Covid!

This is my desk!
I wasn’t sure I could keep working. By the end of a bad day, I could barely move my hands. Sometimes I’d resort to using a pen to click the mouse or keyboard.
I didn’t really know what an RSI was, or how you could get tennis elbow from using a mouse. But I remember asking Dr Google if tennis elbow RSI was permanent. Looking back, it’s hard to say what was worse: the persistent pain of the RSI, or the constant worry it caused.
If any of this sounds familiar, chances are you’ve already been suffering with pain for some time. Take it from me: the sooner you seek medical advice, the better. The longer you leave it, the slower and more complex your recovery will be.
Three years on, I am happy to say I’m in a much better place. Here’s what I learned along the way.
What to expect
First things first: What exactly is RSI?
I’ve just discovered that RSI is not really a thing! Well, not a medical condition, anyway. I’m glad no one told me that 3 years ago.
The term repetitive strain injury (RSI) was coined in 1981 by a non-medical member of the Victorian Trades Hall Council (VTHC). The VTHC defines RSI as:
“an umbrella term for a number of overuse injuries affecting the soft tissues (muscles, tendons, and nerves) of the neck, upper and lower back, chest, shoulders, arms and hands.”
– Victorian Trades Hall Council
There are diagnosable conditions commonly associated with RSI. You may have heard of some of them:
- Bursitis
- Tendinosis (previously called tendinitis)
- De Quervain’s Syndrome (Abductor Policis Longus tendinosis)
- Tennis elbow (Lateral Epicondylitis)
- Golfer’s elbow (Medial Epicondylitis)
- Carpal Tunnel Syndrome
- Ganglions
RSI has also been used to refer to non-specific pain of the upper limbs.
Is RSI the same as OOS?
I’m showing my age. The term RSI has gone out of vogue, mainly because of an “Australian epidemic” of RSI-related WorkCover ‘compo’ claims that happened in the 80s. It’s now called occupational overuse syndrome (OOS) and other less known names. They are basically the same thing.
Statistics from WorkSafe Victoria show that in 2021, body stressing injuries (including OOS) accounted for 36% of all WorkCover claims in Victoria.
Incidentally, I decided early in my treatment not to claim WorkCover. But that’s another story.
Symptoms of RSI
Repetitive strain symptoms can be a bit like mum nagging you to clean your room as a teenager. The first couple of requests are pretty mild, so you pretend not to hear. Once the tone gets a bit more shrill, you reluctantly make a show of tidying until she turns her back. We all know what happens next. Ignore mum long enough and a messy bedroom will be the least of your concerns!
Here are some signs to look out for in the upper limbs:
- Dull ache or throb
- Sharp pain
- Burning or swelling
- Numbness or tingling
- Stiffness, weakness or reduced movement
- Specific areas tender to touch
- Pain that is difficult to pinpoint
For me, the warning signs started several years before the situation got out of hand. Intermittent tenderness in my upper and lower elbows (both sides), occasional wrist pain and some more severe flare-ups.
After some time, I heeded the warning and asked for an ergonomic assessment at work. It helped a little, so naturally, I ignored the recommended exercises.
If there’s anything you learn from this article, let it be to NOT do what I did. Don’t carry on like nothing is happening. See a doctor or physiotherapist. A good one.
My symptoms were eventually put down to nerve compression from a disc bulge in the neck. Specifically, the nerve that travels from the C6 vertebra down the arm to the wrist and hand (thumb to middle finger).
The symptoms had some things in common with Carpal Tunnel.
RSI vs Carpal Tunnel
Carpal tunnel syndrome is just one of the many conditions that fall under the RSI banner. There is usually pain, tingling or numbness that relates directly to compression of the nerve in the wrist. There’s also sleep disrupting night pain, which thankfully, I didn’t have.
Carpal tunnel is commonly associated with office-based work, though direct links are not well established. Repetitive and forceful actions are risk factors. Carpal tunnel can also be misdiagnosed.
That’s the thing about RSI. Symptoms are often similar, so getting a correct diagnosis can be a bit of a process.
What causes RSI?
The cause of RSI is usually a combination of issues. Repetitive movement in your work is often a significant risk. But not everyone who does the same job gets an RSI, so there are likely to be other contributing factors:
- Repetitive actions, vibrations or force sustained over long periods
- Working under pressure
- Poor posture or equipment
- Not taking breaks
- Lack of rest
- Stress
Your underlying health can affect the occurrence or severity of an RSI. General lack of fitness or prior injury, for example.
I ticked all the boxes, and then some. When I look at it now, I was an RSI waiting to happen.
The role of chronic pain and stress
It’s worth mentioning that the complexity of an RSI steps up a notch as soon as you enter chronic pain territory. Chronic Pain Australia describes chronic pain as persistent pain that lasts for over 3 months.
Short-term pain is usually a response to physical damage and disappears once healed. Sometimes, pain persists. It gets a bit screamy, like your mum back there.
The Clinical Director of Viva Physiotherapy, Kathryn Anderson, explains it this way:
“The relationship our brain has with our pain is important, as it tells us when to be cautious and careful. But the longer the nerves and brain are required to do this, the less accurate this messaging becomes.”
– Kathryn Anderson, Physiotherapist
By the time I sought help, my nerves were over-reactive to the conditions of my job, and stress in general. During covid, the niggling disc bulge encountered heightened stress. My entrenched bad habits and posture worsened. Together, they produced more pain. I started stressing about the pain until it became a big bundle of RSI stress, which then turned into chronic RSI pain.
Everything was literally getting on my nerves. By extension, I was getting on everybody else’s nerves.
Once the pain is amplified, it can be more difficult to identify the underlying cause.
Getting an RSI diagnosis
RSI is a pain in the neck to diagnose – literally, in my case.
Chronic pain can be shifty
When I first sought help, my elbow pain was so severe that lifting a kettle was a two-handed job. In the clinic, though, when the doctor performed tests on my arm, the pain would not present. Thankfully, my doctor was kind enough not to make me feel like a hypochondriac.
Tests are often inconclusive
X-rays on my neck and spine showed nothing my physiotherapist couldn’t already deduce – bad posture (a neck like a giraffe), some degeneration (let’s not talk about age) and a touch of scoliosis (who knew!). Ultrasounds on my elbows showed nothing. When an MRI finally produced the culprit, the only person who was unsurprised was my physiotherapist.
For these reasons, doctors often refer to a physiotherapist before ordering any tests. Physiotherapists understand the biomechanics of the body – it’s what they do. They can also liaise with your doctor when further tests are required.
Physical examination
A good physiotherapist will take into consideration your medical history, occupation, and symptoms. They put this together with a physical exam to reveal where the pain comes from and just how sore you are!
In the process, they will find your points of postural weakness and surprise even you with just how inflexible you have become. They will be kind and non-judgmental.
A note about trust
It’s important to trust your physiotherapist. And by that, I don’t mean blind trust because they have credentials. That would be like telling your teenage self to listen to your mother because she’s your mother.
It’s got to feel right. What they say needs to make sense to you. You need to know the treatment is for you, not just any other person who presents with the same symptoms.
I’ll illustrate what I mean.
The occupational therapist who did my workplace ergonomic assessment came across like someone who had been on auto play since the 1980s RSI epidemic. His outlook was as dusty as his exercise diagrams. It could also explain why he saw no reason to replace my 1990s flat-as-a-pancake office chair.
I was never going to do his exercises. Not just because I’m lazy. I had no reason to trust that the exercises he gave were going to work for me.
When I came to Viva Physiotherapy, the contrast couldn’t have been more different. It’s an unfair comparison, of course. He wasn’t there to treat my condition. But you get my point.
What is the best RSI treatment?
The best RSI treatment is one that your physiotherapist tailors to you. Therapy goes hand in hand with diagnosis, so your treatment will change in line with your progress. In the early stages, finding the cause is less important than finding relief.
Relieve RSI pain
The first stage of rehabilitation is what Viva Physiotherapy refers to as the Relieve phase. The aim is to reduce pain so that your focus can turn to healing. If you have persisted with pain for as long as I did, it’s going to take some patience.
RSI Physical Therapy
Who doesn’t like a good massage? Deep tissue massage is one of the hands-on techniques your physiotherapist can use to target the hot spots of your RSI pain. It’s not always pleasant, but it is effective for some short-term relief. You might feel sleepy afterwards.
I organised appointments so they were the last activity of my day before an RDO. It meant I could get an early night, and rest the next day, to maximise the benefit.
Pain medication
Remember what I said about trust? The WorkCover Advisor I consulted (before deciding not to make a claim) advised me to be wary of anyone who suggests pain medication.
I know where she was going with that. There’s the issue of addiction. It’s also probably not the best sign if medication is the primary form of treatment.
When my physiotherapist suggested it could be beneficial, I declined. For a good 9 months. I was determined to work through the pain and let the exercise do its thing.
That was a mistake. Don’t get me wrong. I was making gradual progress with exercise. It just wasn’t proportional to the level of pain.
“While pain medication isn’t a long-term solution for RSI injuries, they can become a useful adjunct to treatment. The clinical challenge we see with RSI is that the slow onset means the issue is quite entrenched before medical help is sought. Medications that act on these different areas can be useful in breaking the cycle of pain to create an opportunity for recovery”.
– Kathryn Anderson, Clinical Director, Viva Physiotherapy
Used as a temporary pain disrupter, medication gave my mind and body a chance to see exercise as a benefit (and not just another irritant). It worked together with exercise to bring the pain down to a background hum. That’s when the real recovery began.
Exercises to Restore function
The Restore phase introduces exercise to help manage pain and improve mobility. For me, gentle stretches started in the first couple of weeks of treatment. Over time, a range of restorative exercises became part of my daily routine. They’re always available whenever I need a quick reset.
RSI neck pain exercises
My physiotherapist prescribed foam roller stretches for neck and back pain. As she explained, pain in one area is often affected by pain or misalignment elsewhere. For me, pain and postural issues in the lower back contribute to nerve compression in my neck.
RSI arm exercises
My nerve pain travels from the neck to the elbows, forearms, wrists, and hands. Stretches for upper limb neural tension are especially beneficial for this kind of pain. Anyone sitting at a computer all day could benefit from these.
Exercises for neck, shoulder, and arm pain
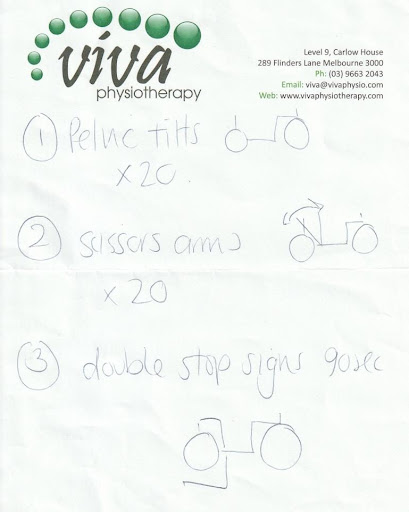
Other exercises offer pain relief with a sneaky bit of core strengthening. I affectionately refer to these as ‘stick figure exercises’ – not a technical term, but the drawings give a pretty accurate depiction of what was going on.
Over time, I incorporated most of these exercises into my working day. Where once my idea of going for a break was a walk to the toilet, I now took a 15-minute break every morning and afternoon to roll about the floor in my trackie dacks. At least lockdown was good for something!
If working in an office is an obstacle for you, try a desk circuit.
You could also talk to your employer. Give them a picture of what floor exercise might look like (see stick figure drawings, above). When I had to return to the office, my coordinator gave me access to the prayer room, so no-one but God had to see my legs in the air.
Yoga for neck and arm pain
Yoga is a recommended treatment for RSI pain. It also has loads of other benefits, including stress relief. I had tried at various times to attend generic yoga classes, only to leave more crippled than I was before. It wasn’t worth the risk.
Viva Physiotherapy was one of the few physiotherapists in Melbourne offering Therapeutic Yoga. The principal, Kath, is also passionate about treating pain. I figured I was in safe hands.
We started out with the basics. Following some one-on-one sessions, I spent two weeks building on each pose:
- Happy Cat, Angry Cat (or in my case, Flat Cat! Seriously, I’m re-watching some of the early videos. My physiotherapist is telling me to arch my back and all I can see is my head moving a tiny bit!)
- Shoulder bridge
- Downward dog
Within three months, I could finally put it all together in a flow. I was ready to join the Therapeutic Yoga class online.
Perform at your best
The Perform phase is all about building resilience. Where Restore retrains muscles you had forgotten or maybe never used, Perform makes them strong. For me, strength training has become the greatest antidote to pain.
Core strength training exercises
Hands up if you enjoy sit-ups? Me neither. The bad news is core strength is key. The good news is you can achieve it without doing 600 sit-ups a day. These mini abs workouts are an accessible entry point. They combine well with learning how to sit actively.
Yoga for strength and flexibility
Yoga is great for people who don’t like sit-ups. Poses are a whole-body experience, meaning your strength and flexibility improve despite you. You might be wobbly at first, or even after 3 years of treatment. But I promise, with proper technique, you will eventually know what it feels like to engage your core.
“The reason for the development of RSI is often multi-factorial. As physiotherapists, we see stiffness and tightness not just in the local tissue, but through the whole body. As such, I often recommend using yoga as a way to address these issues. Many people who’ve had RSI find that initially yoga is tough on their hands and wrists and in fact that weakness is often a precursor that makes that body prone to RSI in the first place. As a physio and yoga teacher, it’s my role to merge these two at a pace that’s right for the injury recovery.”
– Kathryn Anderson, Physiotherapist and Yoga Instructor
Supervised instruction was invaluable for me to learn, safely, the difference between good and bad pain. Now that I am confident, I can enjoy the flexibility of accessing classes from the Viva Hub to practise privately.
RSI strength training
There are a range of options to choose from if yoga is not your thing. You may prefer Clinical Pilates or a combination of exercises to suit your lifestyle. My physiotherapist suggested I alternate yoga with traditional strength training using weights and bands. Something must have worked – I can now deadlift 27kg without injuring myself.
I won’t lie. It was a challenge to go from an infrequent exercise regime to a 5-nights-a-week deal. Initially, the pain was my best motivator – I had no other choice! Now, the exercise is something I want to do because I feel so much better afterwards.
How long does RSI take to heal?
How long RSI takes to heal really depends on your individual situation. How long have you had pain? What are the underlying conditions impacting on your pain? What steps are you willing to take?
I’m the slowest person I know to do most things. Slow to get help. Slow to take pain medication. Slow to embrace core strength exercise. I can’t help thinking if I procrastinated less, my recovery may have been quicker.
The degeneration in my neck is there to stay. Whether pain will continue to be a feature remains to be seen.
What I know is this.
Exercise gives you the chance to prove to yourself that your body can still function even with pain. It has the effect of putting the pain back in its box – you’re pointing at it in the mirror, saying “See? We’re doing this.” As your strength builds, so does your confidence. Pain is no longer in control.
It’s at that point you can imagine a future again.
Where to from here?
After 3 years spent restoring my body to a healthy level of function, am I ready to go forth and conquer the world?
The future looks scary promising. With the encouragement and support of my partner, friends, and physiotherapist, I’m slowly sculpting a new career for myself. One where I am in control.
I’m also looking forward to taking exercise outdoors. Hiking is said to have surprising health benefits. My physiotherapist agrees it’s probably one of the best things I can do for my condition. The Great Ocean Walk is in my sights.
I no longer need pain medication. Before I left my job, I reduced the dosage and stopped completely soon after.
For the first time, I can stand with my shoulders back (and not in a pinch-till-they-hurt kind of way).
Do I still have pain? As I write this, I can feel pain building in my hands. It’s telling me to take a break and do a neural stretch (it really does help, by the way).
Pain is no longer the first or last thing on my mind. It’s more like a companion on my journey, a gentle reminder when I need to pull back. With the tools I now have at my disposal, I’m confident that pain will never rule my world again.
If RSI pain is dominating your life, or even if it’s just a niggle, I hope I’ve given you some encouragement. It can be overwhelming to think of the whole messy picture all at once. So, don’t. Just focus on the one step you can take right now to show your pain who’s boss.
Need help? Kath and her team are kind, compassionate and highly knowledgeable. They can offer advice and support wherever you are on your journey.
References:
Meredith, N. The Australian RSI epidemic 30 years on. Journal of Health, Safety and Environment. 2018; 34 (3): pp.247-259.
Rothmore, P. “Repetitive strain injury: is it real or imagined?” https://theconversation.com/repetitive-strain-injury-is-it-real-or-imagined-21408, 22 January 2014.
“RSI (Repetitive Strain Injury) – What is it?”, https://www.ohsrep.org.au/rsi_repetitive_strain_injury_-_what_is_it, amended July 2020.
“Claims statistical report by calendar year: Claims summary by calendar year from 2022 to 2022”, https://www.worksafe.vic.gov.au/resources/claims-statistical-report-calendar-year, 25 May 2023.
“About Chronic Pain”, https://chronicpainaustralia.org.au/resources/, accessed 21 June 2023.
Butler DS, Mosely G. Lorimer, Explain Pain, Noigroup Publications, 2003.
Kozak A, Schedlbauer G, Wirth T, Euler U, Westermann C, Nienhaus A. Association between work-related biomechanical risk factors and the occurrence of carpal tunnel syndrome: an overview of systematic reviews and a meta-analysis of current research. BMC Musculoskelet Disord. 2015 Sep 1;16:231. doi: 10.1186/s12891-015-0685-0. PMID: 26323649; PMCID: PMC4553935.
Wipperman J, Goerl K. Carpal Tunnel Syndrome: Diagnosis and Management. Am Fam Physician. 2016 Dec 15;94(12):993-999. PMID: 28075090.
Singphow C, Purohit S, Tekur P, Bista S, Panigrahy SN, Raghuram N, Nagendra HR. Effect of Yoga on Stress, Anxiety, Depression, and Spinal Mobility in Computer Users with Chronic Low Back Pain. Int J Yoga. 2022 May-Aug;15(2):114-121. doi: 10.4103/ijoy.ijoy_9_22. Epub 2022 Sep 5. PMID: 36329769; PMCID: PMC9623884.
Garfinkel MS, Singhal A, Katz WA, Allan DA, Reshetar R, Schumacher, Jr HR. Yoga-Based Intervention for Carpal Tunnel Syndrome: A Randomized Trial. JAMA. 1998;280(18):1601–1603. doi:10.1001/jama.280.18.1601
Vitoulas S, Konstantis V, Drizi I, Vrouva S, Koumantakis, GA, Sakellari V. The Effect of Physiotherapy Interventions in the Workplace through Active Micro-Break Activities for Employees with Standing and Sedentary Work. Healthcare. 2022, 10, 2073.
Mitten D, Overholt JR, Haynes FI, D’Amore CC, Ady JC. Hiking: A Low-Cost, Accessible Intervention to Promote Health Benefits. Am J Lifestyle Med. 2016 Jul 9;12(4):302-310. doi: 10.1177/1559827616658229. PMID: 32063815; PMCID: PMC6993091.